- (833) 442-3033
- info@healthclaimexperts.com
- Frisco TX 75034
Professional Credentialing Services for Seamless Provider Enrollment
Ensure your practice stays compliant and fully authorized to deliver care with our end-to-end credentialing support. We handle provider enrollment, contract renewals, CAQH management, and insurance panel applications—so you avoid delays, reduce administrative workload, and focus on patient care while we make sure you’re properly credentialed and ready to serve.
Medical & Insurance Credentialing Services – Provider Enrollment Made Easy
We provide expert medical and insurance credentialing services across the United States. Our team of highly trained and dedicated specialists ensures your practice gets enrolled on insurance panels efficiently and accurately.
From handling complex paperwork to coordinating with insurance companies, we manage the entire credentialing process so you can focus on patient care. With our professional support, you can feel confident that your practice’s credentialing is in safe hands.
What is Medical and Insurance Credentialing?
Credentialing is a process used across various fields, but in healthcare, it specifically refers to Medical Credentialing or Insurance Credentialing. These terms are often used interchangeably.
Healthcare providers — including physicians, hospitals, dentists, chiropractors, physical therapists, occupational therapists, optometrists, urgent care centers, counseling offices, treatment centers, and social workers — who want to bill insurance companies as in-network providers must complete the credentialing process.
This process verifies their qualifications, experience, and professional background, ensuring they meet the standards required by insurance companies and healthcare networks.


Once a provider is credentialed with an insurance company, they are authorized to bill that company directly. Additionally, most insurance panels offer “in-network” providers benefits such as patient referrals and preferential reimbursement rates. Many insurance panels divide the credentialing process into two phases: credentialing and contracting. During the credentialing phase, the panel conducts primary source verification to ensure the provider meets all minimum requirements. Panels may also access CAQH to review the provider’s education and employment history. Once the credentialing phase is complete, the provider’s application moves to the contracting phase. At this point, the provider and their practice may be offered an in-network contract with the insurance panel.
If a provider is offered a contract, it typically includes the fee schedule and the CPT codes they are eligible to bill. In healthcare, the term credentialing often refers to the entire process, covering both the credentialing and contracting phases. Credentialing specialists are trained to manage both phases efficiently, ensuring that providers are accurately enrolled and fully approved on the insurance panels.
Why Medical and Insurance Credentialing is Important
In today’s healthcare market, being able to accept patients’ insurance plans is essential for the success of any medical practice — whether it’s a family clinic, hospital, counseling office, dental or chiropractic practice, physical or occupational therapy center, or optometrist’s office.
If a practice is not in-network with popular insurance plans, patients are likely to choose providers who are, which can directly impact growth and revenue.
While the credentialing process may seem time-consuming and complex, it is a critical step to ensure your practice can serve more patients efficiently. Expert credentialing support helps providers focus on delivering quality care while ensuring timely enrollment with insurance panels.


Our Credentialing Services
Individual Provider Enrollment / Medical Credentialing (Getting on Insurance Panels)
Group Provider Enrollment
CAQH Completion & Management
Primary Source Verification
Hospital Privileging / Medical Staff Credentialing
Recredentialing
Credentialing Appeals
Solo Practices
Physicians
Psychology Counselors
Dentists
Physical, Occupational, and Speech Therapists
Group Medical Practices
Large Medical Centers
Healthcare Facilities
DME Companies
Home Health Agencies

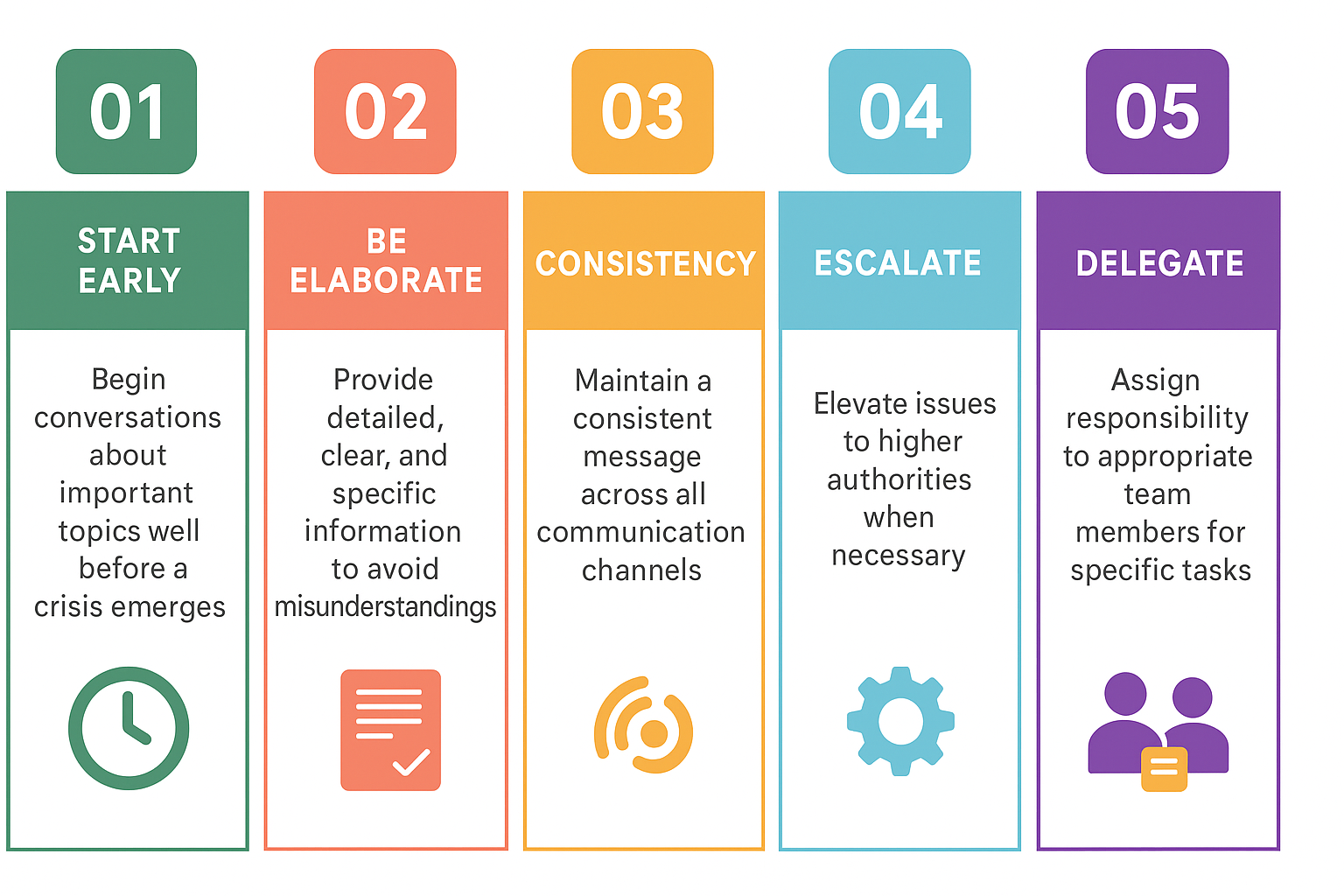
- A Simple 4-Step Credentialing Process
Onboarding
We provide recommendations and assist you in selecting the insurance companies you want to join. You complete our master survey and submit the required documentation.

Application
We gather all current insurance applications and complete them on your behalf within five business days of receiving all required documentation from you.

Follow Up
We follow up to confirm that all applications have been received and proactively ensure the enrollment process progresses smoothly and without delays.

Completion
We notify you of all insurance approvals as soon as confirmation is received and provide all relevant information from the insurance panel. You are then ready to see clients and submit claims for services!
Why Choose Our Professional Credentialing Services?
Rely on a team with extensive experience in insurance credentialing, licensing, and contract negotiations. With years of proven expertise and a strong record of accuracy and reliability, we streamline the entire credentialing process—ensuring smooth approvals, reduced delays, and complete compliance for healthcare providers.

13+ years nationwide experience

Efficient provider network expansion

Working hour availability

Scalable Services

Maintained credentialing calendar

Flexible pricing options
Simplify Your Credentialing Process with Expert Support
Eliminate the stress, paperwork overload, and confusion that comes with dealing directly with insurance carriers. Our credentialing specialists handle the entire process from start to finish, ensuring smooth provider enrollment and compliance at every step. We offer cost-effective credentialing assistance, including primary source verification, for both individual providers and group practices across all specialties.
Whether you need credentialing with government programs or commercial insurance payers, we help you get approved as quickly as possible so you can start receiving reimbursements without delay. Our solutions are designed to fit any type of practice, regardless of size or specialty, and keep you informed throughout the entire process.
Why Medical Credentialing Matters
Medical credentialing plays a crucial role in ensuring patient trust and safety. Through this process, a provider’s education, training, licensure, work history, and professional conduct are thoroughly verified before joining any healthcare organization or payer network. This allows patients to feel confident that their chosen provider meets the required standards of care.
Credentialing is often paired with the enrollment process, which involves submitting applications to insurance networks to be listed as an in-network provider. Together, credentialing and enrollment ensure that healthcare professionals meet all necessary qualifications and can deliver care while receiving proper reimbursement.
List of Provider Medical Credentialing Services
- Comprehensive credentialing solutions for physicians and healthcare organizations
- Revalidation and renewal services for government and private payer programs
- Verification of qualifications for physicians, specialists, and allied health professionals
- Managed administration and coordination of health plan applications
- Outsourced hospital privileging and facility enrollment support
- Contract management for managed care and payer networks
- Consulting services for healthcare organizations to improve credentialing workflows


PROGRAM LIST
OTHERS
Streamline Your Enrollment Process
We handle provider enrollment, CAQH updates, NPI management, and insurance panel applications—so you can focus on patient care.
Fast & Efficient Appointment Coordination
We help clinics manage patient appointments, confirmations, reminders, and scheduling workflows to reduce no-shows and improve efficiency.
Transforming healthcare revenue & empowering providers with seamless billing solutions — where accuracy meets compassion
Quick Link
OUR PROGRAMS
Copyright ©2025 Health Claim Experts . All rights reserved.