- (833) 442-3033
- info@healthclaimexperts.com
- Frisco TX 75034
Reliable Insurance Verification Services for Healthcare Providers
Verifying patients’ health insurance coverage and benefits before delivering medical services is crucial for the financial health of both healthcare providers and their patients. In this article, we explore the importance of insurance verification, its advantages for providers and patients, the risks of skipping this step, and practical strategies to streamline and optimize the insurance verification process in medical practices.
Health Insurance Verification for Medical Practices: Ensuring Smooth and Efficient Billing
Verifying patients’ health insurance coverage and benefits before delivering medical services is crucial for the financial health of both healthcare providers and their patients. In this article, we explore the importance of insurance verification, its advantages for providers and patients, the risks of skipping this step, and practical strategies to streamline and optimize the insurance verification process in medical practices.

Key Benefits of Outsourcing Insurance Eligibility Verification
Insurance eligibility verification is a critical step in the medical billing and coding process. Incorrect or outdated coverage information provided by patients, or a lack of updated data from administrative staff, often leads to denied or delayed claims. These issues can directly impact a practice’s cash flow by postponing reimbursements.
To prevent such problems, many healthcare providers outsource insurance verification to experienced teams who stay current with changes in health plans and policies. Outsourcing ensures efficient and timely verification, streamlines administrative workflows, and helps reduce claim denials and payment delays.
Health Insurance Verification: Why Does It Matter?
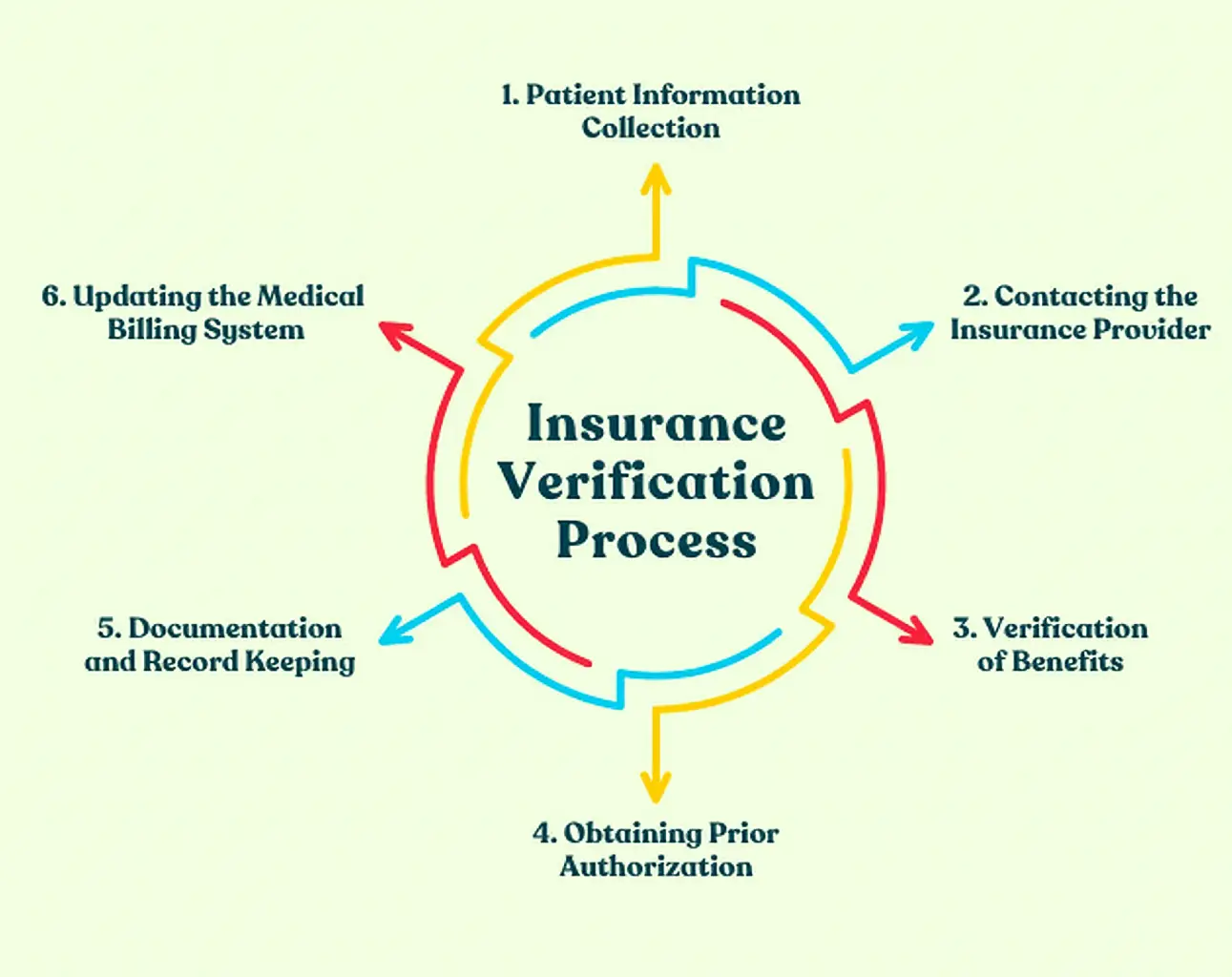
Insurance verification is the process of confirming a patient’s coverage and benefits with their insurance provider before delivering medical services. This essential step helps ensure a smooth billing process, prevents reimbursement issues, and allows medical practices to avoid claim denials, minimize payment delays, and improve overall revenue cycle management.
What Should I Be Aware Of When Doing Policy Verifications?
When conducting policy verifications, healthcare providers should collect all relevant information, including patient demographics, insurance plan details, and specific coverage requirements. It is important to identify any limitations, exclusions, or pre-authorization requirements associated with the policy. Having accurate and up-to-date information is essential for maximizing reimbursements and preventing claim denials.
How Does Insurance Eligibility Verification Benefit Providers?
Insurance eligibility verification provides numerous benefits for medical practices. It allows healthcare providers to confirm a patient’s coverage for specific procedures, ensuring proper reimbursement. By identifying patients with high deductibles or co-pays, providers can discuss financial responsibilities upfront, promoting transparency and reducing billing disputes. Moreover, insurance verification helps streamline the billing process, enhancing operational efficiency and boosting revenue.
Why Is Medical Insurance Eligibility Verification Important?
Health insurance eligibility verification is of paramount importance as it allows healthcare providers to verify a patient’s insurance coverage, ensuring that services rendered are eligible for reimbursement. Failure to verify insurance can lead to claim denials, delayed payments, and increased administrative burdens. By conducting proper insurance verification, medical practices can mitigate financial risks and optimize revenue generation.
What Are The Advantages Of The Insurance Verification Process?
The insurance verification process provides several key benefits:
Reduced Claim Denials: Verifying insurance eligibility lowers the risk of claim denials caused by coverage issues or policy limitations.
Faster Payment Processing: Confirming eligibility and coverage details upfront helps medical practices accelerate payment processing, improving cash flow.
Enhanced Patient Satisfaction: Clear communication about insurance coverage and potential costs builds trust and increases patient satisfaction.
Improved Operational Efficiency: Insurance verification streamlines the billing process, reduces administrative workload, and allows staff to focus more on patient care.
PROGRAM LIST
OTHERS
Streamline Your Enrollment Process
We handle provider enrollment, CAQH updates, NPI management, and insurance panel applications—so you can focus on patient care.
Fast & Efficient Appointment Coordination
We help clinics manage patient appointments, confirmations, reminders, and scheduling workflows to reduce no-shows and improve efficiency.
Transforming healthcare revenue & empowering providers with seamless billing solutions — where accuracy meets compassion
Quick Link
OUR PROGRAMS
Copyright ©2025 Health Claim Experts . All rights reserved.